Understanding Neuropathy: What It Is, Why It Happens, and Why Diabetics Must Pay Attention
If you saw our last video, you may remember Dr. Sam saying: "Diabetes Awareness Month may be over, but diabetes never actually stops. Diabetes can cause something called neuropathy."
Today, we're diving deeper into this critical topic. Neuropathy is one of the most common and life-changing complications of diabetes, yet many people don't know what it really means, what causes it, or how it affects daily life. Dr. Sam is here to break it down in simple, actionable terms.
What Is Neuropathy?
Neuropathy is a broad term that simply means damage or dysfunction of the nerves. Your nerves carry information between your brain, spinal cord, and the rest of your body. When they're not working correctly, a wide range of symptoms can develop.
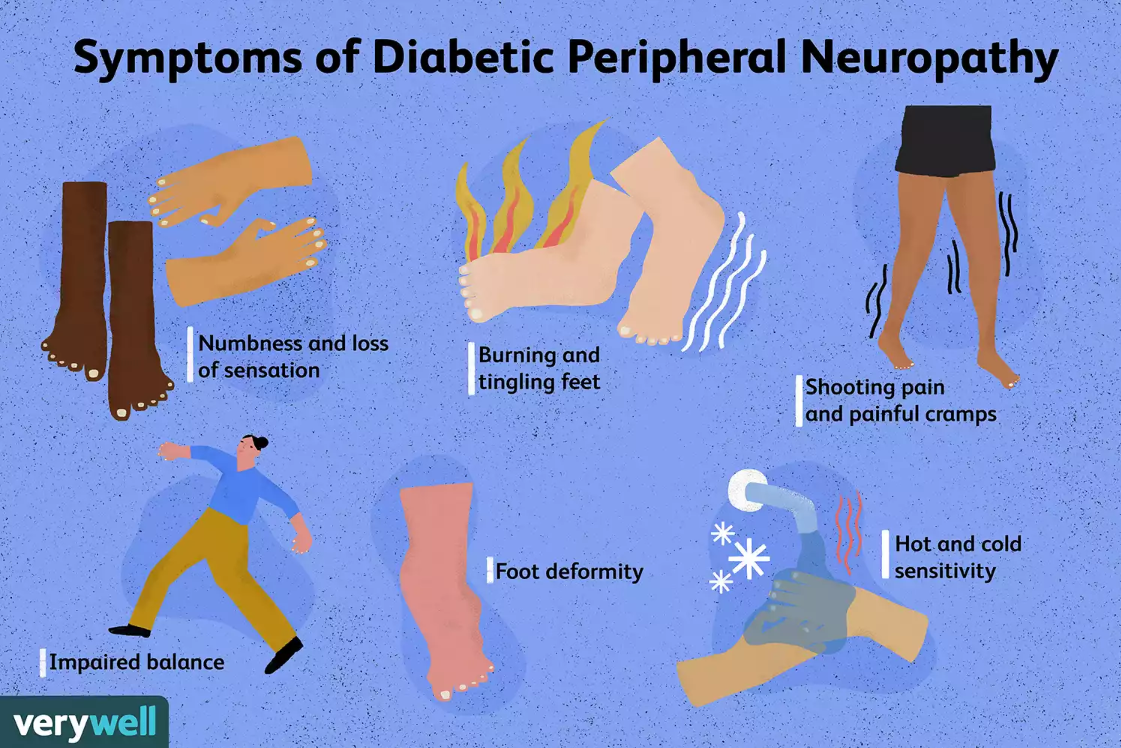
Symptoms can include:
Numbness
Tingling or "pins and needles"
Burning sensations
Electric-shock feelings
Muscle weakness
Changes in skin moisture or sweating
Hypersensitivity to touch
In the medical world, these sensations are called paresthesias.
There are over 100 types of neuropathy, but one of the most common forms is peripheral neuropathy, which affects the feet and ankles most often. According to the National Institute of Neurological Disorders and Stroke (NINDS), neuropathy can be caused by:
Diabetes (the most common cause in the United States) (NINDS, 2020)
Alcohol misuse
Vitamin deficiencies (particularly B12)
Autoimmune diseases
Infections
Genetic disorders
Trauma or injury
In podiatry, diabetes-related neuropathy is the form we see most often.
Why Diabetes Causes Neuropathy
Persistently elevated blood sugar levels damage nerves over time, especially the longest nerves — those that travel to your feet and toes.
Research from the American Diabetes Association shows that up to 50% of people with diabetes will develop neuropathy during their lifetime, primarily sensory (ADA, 2022).
When nerve fibers break down or lose their insulation (myelin), signals become distorted or lost. This leads to the various symptoms mentioned above, particularly loss of protective sensation in the feet.
The Three Main Types of Neuropathy
As Dr. Sam explains in the video: "In the foot and ankle world, we focus a lot on diabetic neuropathy. For some reason, your nerves are not working the way they should. There's actually multiple types of neuropathy."
Different nerves control different types of functions, which is why there are multiple forms of neuropathy:
1. Sensory Neuropathy
Sensory neuropathy is the most common form seen in diabetic patients. It affects the nerves responsible for feeling and sensation in your feet and hands. Key symptoms include:
Tingling or burning sensations
Numbness in the toes or soles
Heightened sensitivity to touch (allodynia)
Loss of ability to feel temperature, pain, and touch
Sensory neuropathy is particularly concerning because it reduces protective sensation, making it easier for injuries or ulcers to go unnoticed. According to the American Diabetes Association, up to 50% of diabetic patients develop peripheral neuropathy, primarily sensory (ADA, 2022).
2. Motor Neuropathy
Motor neuropathy is less common and affects the nerves that control muscle movement. While diabetes is a cause, motor neuropathy often results from trauma, injury, or other systemic conditions. Potential impacts include:
Weakness in foot muscles
Instability while walking
Changes in foot shape (e.g., hammertoes)
Balance problems
Motor neuropathy can increase the risk of falls and musculoskeletal injuries, making early recognition and treatment essential (Tesfaye et al., 2011).
3. Autonomic Neuropathy
Autonomic neuropathy affects the involuntary functions of the body, like sweating, circulation, digestion, and blood pressure regulation. In the feet, this often leads to:
Dry skin due to reduced sweat production
Cracked heels or fissures, which increase the risk of infection
Occasionally, excessive sweating (hyperhidrosis)
Dr. Sam explains that dry skin caused by autonomic neuropathy is not just uncomfortable; it can also create cracks and wounds that are prone to infection, even in non-diabetic individuals. Proper moisturization and monitoring are key, but underlying nerve damage must also be addressed.
Most diabetic patients experience a combination of these types.
Why Neuropathy Is More Serious Than You Think
Neuropathy isn't just uncomfortable; it can be painful, disruptive, and dangerous. It not only reduces quality of life but also increases the risk of foot ulcers, infections, and even amputations if left untreated. Because neuropathy causes loss of protective sensation, small injuries go unnoticed. This can lead to:
Foot ulcers
Infections
Delayed healing
Higher risk of amputation
Persistent burning, tingling, or numbness
Skin changes like dryness, cracking, or infections
Reduced mobility and balance issues
A major multicenter study found that diabetic neuropathy is the strongest risk factor for foot ulceration (Armstrong et al., 2017). This is why preventive foot exams are essential.
How Neuropathy Impacts Daily Quality of Life
"Some people can't have anything touching the area, because it causes them so much discomfort." -Dr. Sam
Neuropathy can affect:
Walking
Balance
Sleep
Work
Enjoyment of daily activities
And because symptoms worsen over time, early evaluation and management are crucial.
What Can You Do?
Get a comprehensive diabetic foot exam
Even if you don't feel symptoms, annual foot exams by a podiatrist or healthcare professional can catch problems early. At least once a year—more often if you already have neuropathy (CDC, 2023).
Control blood sugar levels
Maintain blood sugar, nutrition, and overall health to reduce nerve damage progression. This is the #1 way to slow nerve damage (ADA, 2022).
Monitor your feet daily
Check for cracks, redness, swelling, or changes in sensation.
Report new symptoms early
Burning, tingling, numbness, or sudden changes are not "just part of diabetes."
Moisturize carefully
Use lotion on dry skin but avoid applying between toes to prevent fungal infections.
Wear protective footwear
Neuropathy makes injuries easy to miss.
Seek professional care - Schedule an appointment with Dr. SAm
If you experience numbness, tingling, burning, dry skin, or any unexplained foot changes, come see us at AM Physicians. Early intervention can prevent complications and improve quality of life.
Especially if you have ulcers, infections, or balance problems, get a care plan by scheduling an appointment with Dr. Sam.
Bottom Line: Diabetes Doesn't Stop, And Neither Should Your Foot Care
Diabetes Awareness Month may be over, but diabetic foot care is a year-round necessity.
Neuropathy is a complex condition with sensory, motor, and autonomic components. Whether caused by diabetes or other factors, it requires attention, monitoring, and care. It can start silently and progress quickly. Understanding your symptoms and seeking help early can prevent life-altering complications. Taking neuropathy seriously today can protect your mobility and health tomorrow.
Dr. Sam and the AM Physicians team are waiting for you.